Diagnosing Colorectal Cancer Earlier
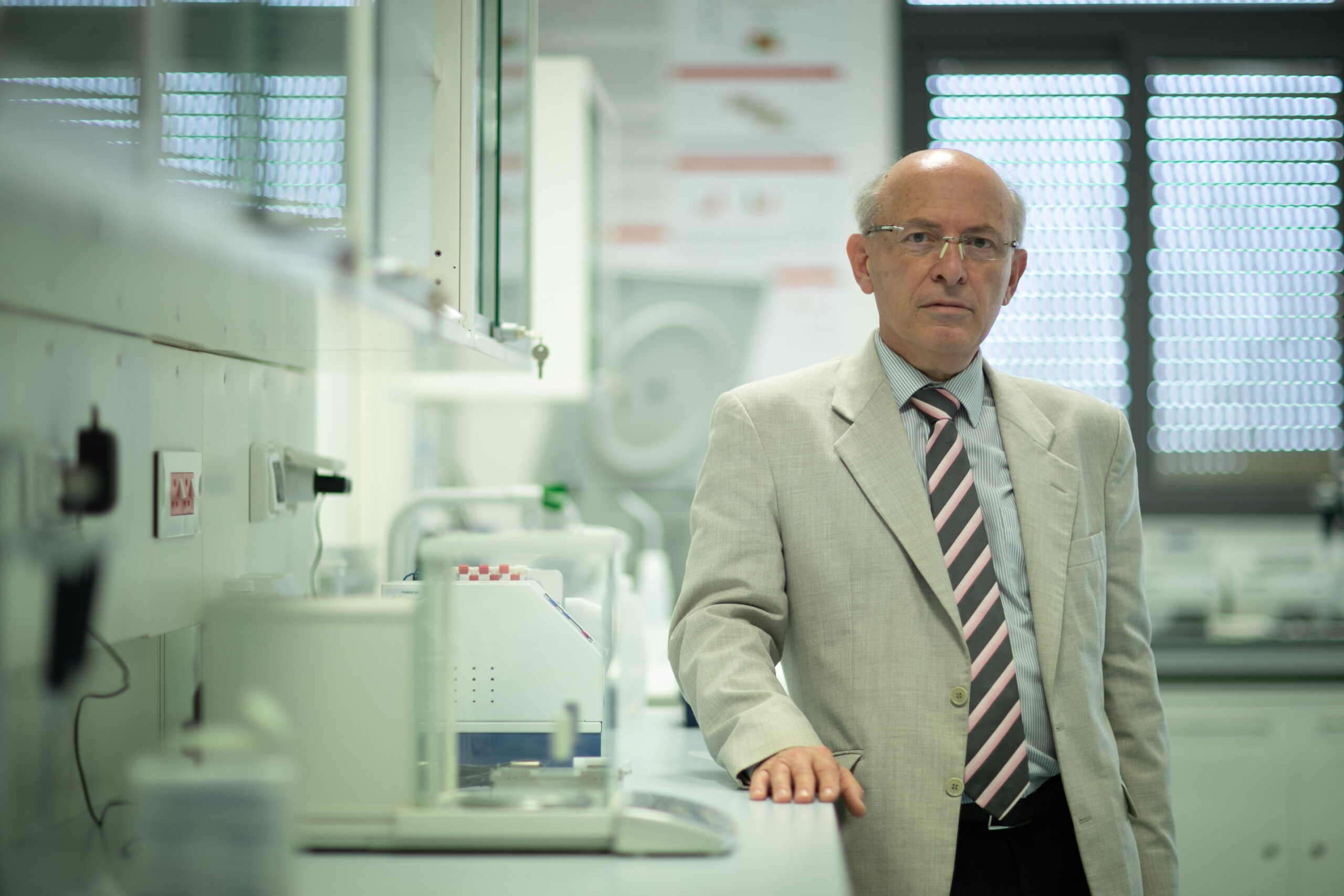
The ‘Colorectal Cancer Risk Factors and Design of Preventive Strategy and Early Diagnosis’ project is led by Prof Godfrey Grech from the Faculty of Medicine and Surgery, Department of Pathology at the University of Malta, in collaboration with Prof Godfrey LaFerla.
In Malta, colorectal cancer (CRC) is the second most common type of cancer in terms of new cases and deaths. Also known as bowel cancer, colon cancer or rectal cancer, CRC is the development of cancer from the colon, rectum or parts of the large intestine.
Most CRC cases are due to age or lifestyle factors, while few are linked to underlying genetic disorders. However, the lack of early symptoms, coupled with low acceptability towards screening programmes or medical advice, means that many CRC cases are diagnosed at an advanced stage of the disease. By contrast, early diagnosis often allows for more treatment options, a better quality of life – and a higher chance of survival.
This new project from the University of Malta hopes to offer more scope for the early diagnosis of CRC, while determining the risk factors behind the disease and even designing a strategy for preventing it.
“We set out to create a fully-comprehensive, sampled prospective cohort study, where we would follow a group of similar individuals with key differences over time, to observe how they are each affected,” explains Prof Grech. “Our pilot project would measure microbiome profiles and plasma biomarkers, providing us with high quality data upon which to design a potential future strategy for early diagnosis.”
The discovery of a blood test that offers early detection of CRC may have significant impact globally. It may inspire a wider acceptability for screening, which increases the chances of establishing more effective treatment outcomes for the patient.
Meanwhile, previous studies have shown a correlation between gut bacteria composition and colorectal cancer. With this connection in mind, the project has also been designed to associate gut microbiota with specific dietary intake and compare these findings alongside the progression of disease.
“The balance of gut bacteria is highly affected by diet. Their diversity and abundance have a major role in gut lining integrity, complex metabolism of dietary components, and inflammation and immune function,” Prof Grech elaborates. “Since microbiota composition can be measured as part of a screening process utilising a faecal sample, understanding the correlation could mean understanding how the disease progresses – and diagnosing it earlier.”
Preliminary studies involved collection of dietary information and staining of fixed tissue with proliferation markers. Through this process, the team noticed that a certain proliferation marker was increased in the early stages of the disease, which was associated with a high fat, high protein, low fibre diet. The finding prompted the team to explore other forms of proliferation markers in plasma samples, to record their effects.

In addition, a blood sample was taken from consenting individuals to isolate exosomes in blood to investigate the possibility of an increase in proliferation markers.
“The use of blood-derived exosomes could be a potential method to screen this change originating from tissues,” continues Prof Grech. “We have shown that exosomes can be isolated from metastatic CRC patients and that gene amplification found in cancer tissue is measured in blood-derived exosomes.”
Once microbiota data is analysed and the results originating from plasma correlated with dietary findings, the project is set to join a more international effort against CRC.
“This project will provide the basis of a prospective study in collaboration with the International Agency for Research on Cancer (IARC-WHO), which established and coordinates the large EPIC (European Prospective Investigation into Cancer and Nutrition) cohort,” concludes Prof Grech.
This project received €60,000 from the RIDT in 2019 under the ALIVE Cancer Research Grant.